Abstract
In-situ vaccination is a local intervention in which immune enhancing agents are injected locally into one site of tumor, triggering a T cell immune response locally that then travels to attack cancer throughout the body.
We have employed a preclinical strategy whereby the same syngeneic tumor is implanted at two separate sites in the body. One tumor is then injected with the test agents and the resulting systemic immune response, if any, is detected by the regression of the distant, untreated tumor.
In this test for abscopal therapeutic effects, the combination of unmethylated CG-enriched oligodeoxynucleotide (CpG) - a TLR9 ligand - and agonist anti-OX40 antibody has provided impressive results. This combination lead to durable disease control and long-term treatment-free survival in multiple mouse models of cancer. CpG induced myeloid cells to secrete cytokines, which subsequently induced OX40 expression on T cells.
Thus, we hypothesized that administration sequence and timing may affect the anti-tumor responses of in-situ vaccination.
In order to screen for the best sequence and timing we implanted A20 lymphoma tumors bilaterally in opposite sides of the abdomen of Balb/C mice. After tumors were established, one tumor was injected at the selected sequence and timing with the test agents and the resulting immune response was monitored by the measuring growth of the distant, untreated tumor.
As opposed to our usual schedule of three injections, even a single injection of CpG (50µg) and anti-OX40 (8µg) resulted in a fully protective systemic immune response. In addition, the cured animals were protected from re-challenge with the same A20 tumor but not unrelated tumors.
Decreasing the dose even further to 10µg CpG and 1µg anti-OX40 partially preserved the therapeutic response with a long-term survival of 60%. Concurrent administration of CpG and anti-OX40 resulted in eradication of both local and distant disease. Sequential administration of CpG followed by anti-OX40 preserved the therapeutic efficacy. However, the opposite order of anti-OX40 followed by CpG significantly attenuated the therapeutic effect. While CpG followed by a 24- or 48-hour-delayed anti-OX40 treatment preserved the therapeutic efficacy, a 72h delay in anti-OX40 administration resulted in reduced therapeutic effect.
These data demonstrate the importance of the administration sequence for fully protective anti-tumor immune responses. Our data suggest that the anti-OX40 antibody should be administered at the same time as CpG or with only a slight delay but not in the reverse order.
Low-dose radiotherapy (2×2 Gy) is an effective treatment for patients with indolent non-Hodgkin's lymphoma. This treatment results in high response rates at the treated site. Since immune infiltrating cells in the tumor microenvironment are essential for in situ vaccination of CpG and anti-OX40 we aimed to assess the effect of adding radiation in our pre-clinical models of lymphoma. We found that the addition of 2x2 Gy radiation did not interfere with the induction of a protective immune response by of CpG and anti-OX40.
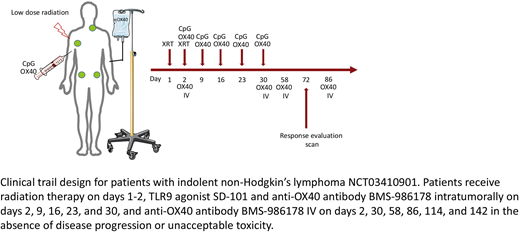
Given the effectiveness of low dose radiotherapy for local control and its lack of interference with the immune related abscopal response in the pre-clinical model, we are including radiation in our current clinical trials. In addition, we have incorporated our findings in the preclinical model regarding dosing and scheduling of CpG and anti-OX40 antibody to the design of our current in situ vaccination lymphoma clinical trial.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal